What is a dental implant?

A dental implant is a screw, usually made from titanium, that is used to replace the root of a missing tooth. The implant is screwed into the jaw where it provides a solid foundation for a crown, bridge or other dental prosthesis that replaces one or more missing teeth.
What is osseointegration?

After an implant is placed, the surrounding bone will grow in contact with the implant surface and attach to it. This process of attachment is called "osseointegration". If osseointegration is not established or is lost, the implant will become loose and fail.
What are dental implants for?

Implants are used to fix a crown, a bridge, or a prosthesis that replaces one or more missing teeth. The aim is to improve your health, chewing function and/or aesthetic appearance.
I am allergic to titanium Can I still have dental im-plants?

Dental implants are normally made of commercially pure titanium. Allergy to titanium is rare and very few cases have been reported. If you are allergic to titanium, it may be possible for you to have an implant made of another material that will be accepted by your bone and osseointegrate.
How long do implants last?

Implants have high success rates and there are reports that have assessed their performance over a period of more than 35 years. The most recent studies indicate that 90 percent of implants placed ten years ago are still functional today. The long-term success of implants also depends greatly on how well they are cleaned and maintained. In most cases, as a minimum, an annual check-up is likely to be recommended so the implants can be professionally cleaned by your dentist or hygienist. Moreover, brushing and flossing twice a day is essential for their long-term survival.
Are implants painful?

No. An effective local anaesthetic is used before surgery so no discomfort is felt as implants are placed. Any mild discomfort that may be experienced after surgery can be controlled with conventional painkiller tablets.
What are the potential complications of dental implants?

Several complications may be encountered, but they can all be managed effectively:
1. Bone loss
Bone loss can occur around implants. Regular check-ups by your implant dentist will ensure that any more extensive bone loss is spotted and treated.
2. Infection
Infections around implants mostly result from poor oral hygiene. To prevent infections, implants should be professionally cleaned by your dentist or a hygienist on a regular basis. If you are a periodontal patient you should also follow a program of preventive periodontal therapy.
I am a periodontal patient. Can I have dental implants?

Yes, periodontal patients can have dental implants. However, it is important that periodontitis affecting your remaining natural teeth is adequately treated before implant placement. It is also important to note that the risk of complications related to implant treatment seems to be somewhat higher in periodontal patients.
I have lost my tooth/teeth due to periodontal disease, are dental implants still an option?

Yes, implants may also be a suitable treatment option if you have lost teeth due to periodontal disease. However, prior to implant treatment it is important to treat the periodontitis affecting the remaining teeth.
Can periodontal infection, affect dental implants?

Periodontal disease affecting natural teeth may increase the risk of infection around dental implants. Therefore, it should be treated before implant placement.
What are peri-implant diseases?
Peri-implant diseases are often compared to periodontal diseases that affect natural teeth. The initial inflammation of the mucosa surrounding a dental implant is termed peri-implant mucositis. This inflammation may be reversible if adequate treatment is provided. If the soft tissue inflammation is accompanied by loss of bone around the implant, the condition is termed peri-implantitis. Treatment of this condition must be managed by your periodontist and their team.
Can peri-implant diseases be treated?

Yes, peri-implant diseases can be treated. If bone loss is identified at the inflamed site(s), it is often necessary to perform surgical interventions to re-establish healthy conditions.
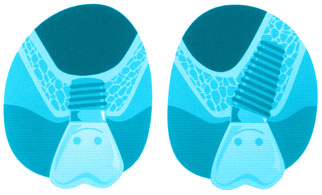
How should I clean my dental implants?

Dental implants are basically cleaned in the same way as your natural teeth. However, it is particularly important to clean in between the implants or between remaining teeth and implants. Special interdental brushes may be used to facilitate this, along with dental floss.
How often, should I go to my dentist to have my teeth cleaned after getting dental implants?

Your dentist will put together a maintenance program that is appropriate for your individual needs. As a minimum, an annual check up is likely to be recommended, but supportive periodontal therapy every three months could be necessary if you have had tooth loss due to periodontitis.
Will smoking affect the success of my dental implant treatment?

Smoking increases the risk of implant complications, just as it increases the risk of periodontitis around natural teeth. Smoking cessation is recommended before implant treatment takes place in order to assure a better treatment outcome. However, implants can be successfully placed in a high percentage of patients who smoke.
Am I a suitable candidate for dental implants?

Most people who are in good general health, or with systemic diseases that are under control are good candidates for dental implants.
Are dental implants ever contraindicated?

Implants are rarely contraindicated, However it may not be possible to receive dental implants if you are taking specific drugs or are medically compromised.
Will I experience pain after the implant is placed?

Any mild discomfort that may be experienced after surgery can be controlled with conventional painkiller tablets.
Are there any surgical risks when implants are placed?

As with all treatment procedures, there is a degree of surgical risk when an implant is placed. The likelihood of a risk occurring depends on a range of factors, including the area being treated. Minor risks are in most cases transitory and can be controlled. They include hematoma, bleeding, swelling, pain or discomfort. There are very few major risks associated with implant surgery and although they can potentially occur, they are extremely rare.
What is the healing time for implants?

Generally, implants require a healing time of two to four months before placement of the prosthesis. Under specific circumstances and following well established protocols, implants may be restored (have a prosthesis placed) on the same day the implant is inserted. This is known as immediate loading.
What is an immediate implant?

An immediate implant is a surgical procedure in which the dental implant is positioned during the same appointment that the tooth is extracted.
Will I have a temporary crown, bridge or removable prosthesis while my implant is healing?

Yes, this will be possible in most cases. A temporary crown or bridge may sometimes be attached to the implant(s) during the healing period. Alternatively, a removable prosthesis may be the temporary treatment of choice.
During the treatment will I be able to continue en-joying all the activities I would normally do?

Yes. Although sports and other vigorous activities are best avoided for the first one to two weeks after surgery.
Can dental implants help improve my smile?

If you have lost one or more front teeth, dental implants are an excellent treatment option that can help improve your smile. In most cases crowns on dental implants look very natural, just like your real teeth. Normally, people will not realize that what you have is actually an implant-supported crown. Dental implants attach to the bone and stay fixed in position allowing you to smile comfortably and naturally.
What happens to the gingiva and the jaw bone after a tooth is lost?

Immediately after a tooth is removed, a blood clot forms in the socket. Over the following weeks, blood vessels and cells from the socket wall form bone, repairing the socket. At the same time, gingival cells migrate across the surface of the blood clot creating new gingiva and closing the extraction socket. Unfortunately, healing of the socket is normally associated with shrinkage and reduction of both bone and soft tissue.
The extent of the tissue loss depends on a number of factors including your individual biology and the degree of tissue trauma during the removal of the tooth.
Can the loss of tissue after a tooth is extracted be prevented?

The loss of tissue following tooth extraction can be minimized by limiting the trauma to the bone and soft tissue, and by avoiding removal of bone during the extraction. Sometimes the empty socket is filled with a bone grafting material immediately after extraction to minimize loss of tissue.
Can lost bone be reconstructed?

Lost bone can be reconstructed in various ways. This includes using autogenous (your own) bone tissue. The process generally involves removing bone from a second surgical site, and as a result it is associated with the risk of additional morbidity. There are other types of bone grafting materials (bone substitutes) that can be used.
All grafting materials have to be integrated into the recipient site by penetration of newly formed bone which originates from the underlying jaw bone. Autogenous grafts have a biological activity of their own through the bone cells and bone matrix that is transferred. Other grafting materials are devoid of biological activity and rely on the ability of the residual bone tissue to incorporate them. The extent of bone loss, the location of the bone defect, and the condition of the overlaying soft tissues will have an impact on the material and technique of choice.
I have been told that I need a sinus lift. What is this?

A sinus lift is a surgical procedure that elevates the inner lining of the maxillary sinus. This creates a space between the maxillary bone and sinus membrane into which bone grafting material is placed. A sinus lift is often necessary within the molar and bicuspid areas of the upper jaw because the bone height is reduced after the bicuspid and molar teeth are lost. As a result, the bone height needs to be restored before implants can be placed. Where the loss of bone height is limited, a sinus lift can be performed through the socket that is prepared for the implant. Where bone loss is more extensive, access to the sinus membrane is required through the lateral sinus wall to allow for a controlled and safe elevation of the membrane. Sometimes implants can be placed at the same time as the sinus lift procedure is performed.
What are the alternatives to a sinus lift?
Alternative approaches are the use of short implants that can be placed in the residual bone underneath the sinus membrane. Another option is the use of angulated implants that are placed into the triangular bone contour in front of and behind the sinus membrane.
I am diabetic. Can I have dental implants?

Yes, diabetes is not a contraindication for implant therapy. However, diabetes should be well controlled before treatment commences. In addition, your dentist may give you antibiotics to avoid any risk of post-operative infection. Sometimes your dentist will also recommend that the healing period is extended (the time between the implant is placed and the prosthetic work begins).
I am using bisphosphonates for my osteoporosis. Can I have dental implants?

In most cases you can have implants if you are taking oral bisphosphonates. International consensus conferences have concluded that there seems to be no need to stop oral bisphosphonates treatment before implant placement. However, intravenous bisphosphonates are an absolute contraindication for any oral surgery.
I am taking anticoagulant medication, Can I have dental implants?

Anticoagulant medication is not generally a contraindication for simple oral surgery, including implant placement. Advanced surgeries including bone and soft tissue grafting can be performed after consultation and with the consent of the general physician where anticoagulant treatment is likely to be temporarily stopped or modified.
Can I have dental implants while I am pregnant?

Oral surgery is not recommended during pregnancy, even though implant surgery is generally very simple and without complications. However, some complications can potentially arise with the need to prescribe antibiotics and/ or anti-inflammatory medications. As a result it is best to avoid implant surgery during pregnancy
I have cardiovascular disease. Can I have dental implants?

There are only a few absolute contraindications that relate to cardiovascular diseases. For example, implant placement cannot be considered within six months of a heart attack. Also, for any cardiovascular pathology, implant surgery can only be performed with the authorization of your cardiologist. Medical recommendations may vary depending on the country you live in.
I have osteoporosis.Can I have dental implants?
Yes, osteoporosis is not a contraindication for implant placement. Several scientific studies have compared implant survival among patients with osteoporosis and those without. No differences were found. However, one of the treatments for osteoporosis is bisphosphonates, which need to be taken into account when considering treatment.
I am over 80 years old. Can I have dental implants?

Yes, there are no contraindications to placing implants in patients over 80 years of age. No increase in the rate of failures has been reported in most cases. If you have no other contraindications for oral surgery, you can have implants.
I am a teenager and have a broken tooth, Can I have dental, implants?

Dental implants are only appropriate when facial growth is complete. If a dentist places implants too soon, there can be adverse cosmetic results when facial growth is complete. Your dentist will identify the most effective interim solution that allows implant placement to be performed at the right time.
